Improved Diabetes Management For Inpatients
After research showed that 33% of inpatients at KEMH have diabetes, the Bermuda Hospitals Board [BHB] is working to improve care for diabetic patients.
A spokesperson said, “BHB is focusing on improving inpatient care for diabetic patients, after internal research showed that 33% of inpatients at KEMH have diabetes. Irrespective of the primary cause of their admission to hospital, patients with diabetes are known to have poorer outcomes and longer hospital stays because of their diabetes.
“Dr Andrew Jamieson, Endocrinologist, leads BHB’s Diabetes, Respiratory, Endocrinology and Metabolism [DREAM] Centre, and is overseeing this new focus of care.
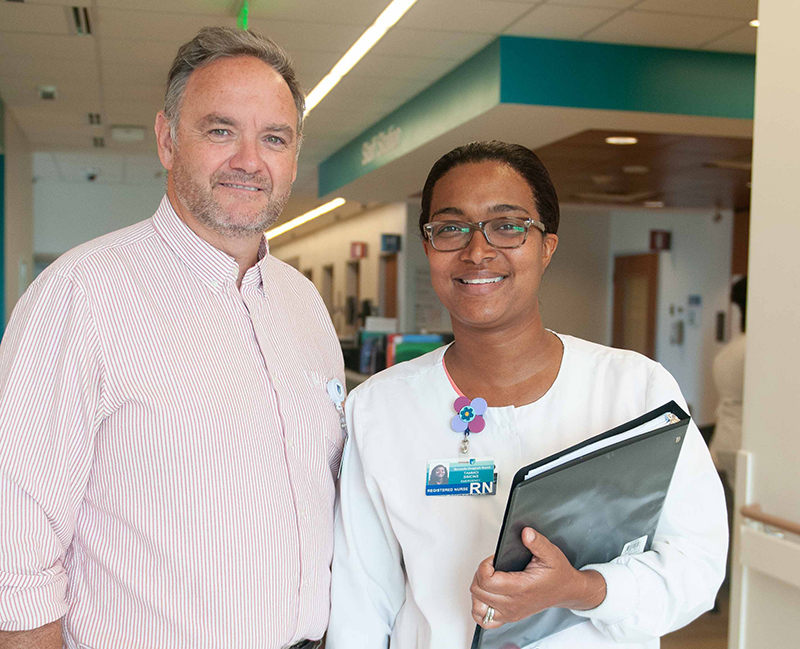
Dr Andrew Jamieson, BHB Endocrinologist, and Registered Nurse and Diabetes Educator, Tammoi Simons
Dr Jamieson notes: “By optimizing blood sugar control in hospital, many studies have shown that one can improve quality of care for patients with wounds, infections, as well as heart disease and stroke.
“We are particularly keen to do our part in supporting the hospital’s new stroke service going into the future as, on average, 40% of patients with stroke have diabetes. We want to help people manage their diabetes, return to their homes sooner and improve their wellness and quality of life. Over the longer term this means people with diabetes experience fewer complications, and overall this helps reduce healthcare costs for individuals and the island as a whole.”
The intensive focus on inpatient care includes daily rounding of most patients with diabetes by Dr Jamieson with Diabetes Nurse Educator, Tammoi Simons. That translates to about 30 patients in the Acute Care Wing each day. Ms Simons undertook the inpatient research on inpatients and focuses on patient education.
She said, “It is staggering to know how many people in hospital have diabetes. We can make a huge difference by reaching them while they are in our care. Our new daily rounding for diabetes gives us time to help patients understand their diagnosis and how to use their medications before they leave hospital.
“This reduces the chances that patients with diabetes are readmitted simply because they do not understand how to use insulin or other medications. We are also arranging up rapid response follow-up after their discharge with the DREAM Centre staff. ”
This new fast track system provides early support at the BHB’s DREAM Centre for patients who are discharged from the wards or from the Emergency Department.
Dr Jamieson explains: “If we can arrange appointments with the DREAM Centre we can help support an early discharge and give people the support they need to improve their lives. Patients who are diagnosed with diabetes in the Emergency Department or in hospital often require rapid transition to a comprehensive outpatient care once they are discharged from hospital. This is so that they can receive multi-disciplinary preventative care which is critical in preventing readmission, and controlling diabetes as well as avoiding complications in the first place.”
Dr. Jamieson is working on a new protocol for critically ill patients with diabetes and is working with Ms Simons to provide educational services for hospital staff, both nurses and physicians, who also manage patients with diabetes in the hospital.